I want to discuss COVID testing this school year. It’s surprisingly complex.
Depending on where you live and how school are approaching pandemic policies your children may be getting tested routinely. This is a fantastic way to identify children with COVID who may be free of symptoms (which HALF are) and not identified by temperature screening, check-lists, or exposure history. The drawback is that when the incidence of COVID-19 drops below a certain level in your community, routine testing will identify more false positives (where a child tests positive, but doesn’t have COVID-19) than true positives. If you are curious about this or involved in a school’s plan for testing, you can play with the calculator here.
But for the rest of the parents who are faced with the decision about when to test, it feels complicated because it is complicated. The goals of testing your child are numerous.
You want to know when your child has COVID-19:
To monitor their illness and recovery.
To keep them from infecting others including your household, school, and workplace communities.
It’s worth acknowledging that we also don’t want to over-test or test too frequently for COVID-19.
It’s expensive, inconvenient, or uncomfortable.
You risk identifying false positives and creating unnecessary panic and restriction for yourself and others.
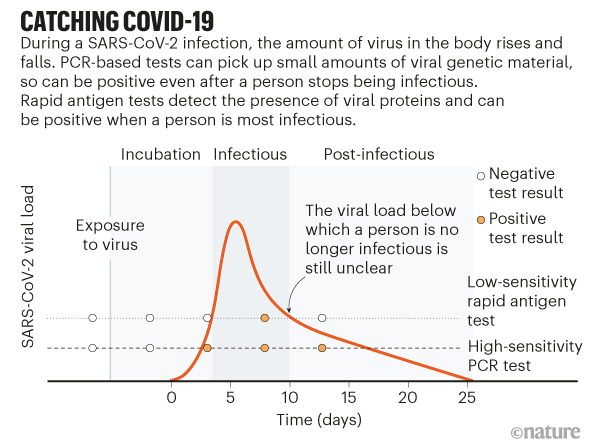
When your child is not feeling well, you want to test right away because you want to notify individuals who may have been exposed. However, we know early in illness, you do run the risk of testing negative, but actually having COVID-19. The timing of the test depends on which test you have access to and turnaround time of the test locally. In an ideal world, I would test the first day. If the child tests negative but is still sick I would repeat the test day 3-5.
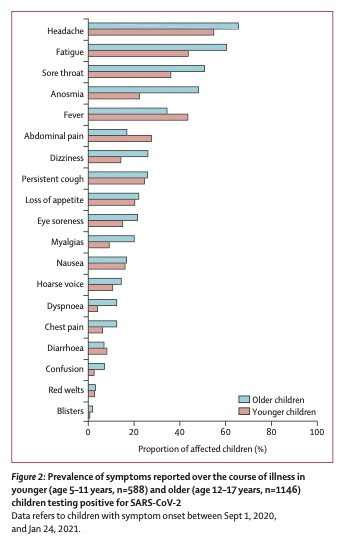
The most common symptoms children experience are very nonspecific, this chart is from the recent Lancet article reflecting UK experience 9/1/20-1/24/21 (pre-delta).
My strategy would be to test whenever your child is sick and unable to attend school. I use a common sense approach to this, but your school may have different rules so you have to know and follow the local guidelines. If my children have 1 major symptom including fever, shortness of breath OR anosmia, I would keep them home and test. Additionally if my children had 2 minor symptoms including any from the chart above, I would keep them home and test. Severity is another metric to consider. Any child who has mild seasonal allergies or a significant tantrum or crying spurt, may have a runny nose. Runny noses can persist for 4-6 weeks following viruses, so we also have to take history into account when evaluating minor symptoms.
When your child is ill, what sort of test you use doesn’t matter as much. In the US, there are several good over the counter tests to consider. If you need a report, you’ll likely need to involve a doctor. Many antigen tests are approved for over the counter use and these are the three I’ve seen most.
the Ellume (96% sensitive when compared to PCR)
the Sofia Quidel (80% sensitive when symptomatic) and
the Abbott Binax now (71-88% sensitive when symptomatic depending on which study you read, perhaps due to temperature sensitivity or swab quality).
You can also consider repeating antigen tests to increase their sensitivity, this is why the Abbott Binax and the Sofia Quidel tests are sold in a two pack with instructions to take 2 tests separated by 24- 36 hours.
Of these options, I prefer the Ellume, but we have seen some false positives (child tests positive, but same day PCR is negative). If you are considering testing at home, it’s worth understanding what determines the risk of false positive because the biggest factor is the incidence of COVID-19 in the population being tested (this math is from an FDA report).
If 10% have COVID-19, only 20% of the positive results would be a false positive.
If 1% have COVID-19, 70% of the positive results would be false positives.
If 0.1% have COVID-19, 96% of the positive results will be false positives. Yes only 4/100 will be true positives.
So, I recommend if the test is positive to quarantine AND confirm with a PCR.
The Lucira uses technology more similar to PCR and when it’s back in stock represents the best option. If you do use one of these home tests, be sure to read and follow the instructions precisely to maximize the sensitivity of your results. I have no conflict of interest, affiliate links, or kickbacks in making these recommendations.
Now what about testing when your child is well? When your child is not showing any symptoms, you may choose to test in then following scenarios.
Your child is quarantining after an exposure. While it’s nice to test right away and know sooner, the most reliable results are at least three and probably 5 days after exposure.
You are returning from a vacation where you took more exposure risks than normal and want to be considerate of your workplace or school.
You are going to see someone who is medically fragile (ie. your grandfather who is on chemotherapy and hasn’t developed antibodies despite COVID vaccination) and you want to minimize their risk.
It’s well established that when you do not have symptoms, the antigen based over the counter tests may not work as well as PCR tests. Only the Ellume received FDA approval to be used in asymptomatic individuals. In one study, the Sofia test mentioned above only identified 32% of individuals who were positive for COVID and asymptomatic.
Some physicians would say that the difference may be in the cut-off. When the PCR has a low cycle time threshold indicating higher viral levels, the antigen tests do better. This implies that the antigen tests may catch the asymptomatic people most likely to be infectious towards others that matter the most.
It’s also worth noting that most of this data comes from the original strains of COVID, not delta, which we know is present in higher quantities in those who are infected. This may mean that antigen tests are more useful now than we previously thought.
Any test is a snap shot in time. So the accessibility of the testing matters. If you are testing before seeing a high risk loved one and you can take a rapid antigen test that day, it may be imperfect, but your result will represent your risk that day. If the alternate plan is to take a PCR three days prior to the visit and wait for results, your result is more reliable, but the gap of 3 days may lead you to miss a new infection. There is value to having the test right before you see your loved one.
While I tried to write this to help clarify a strategy about testing this school year, I realize that I may have confused you further. It’s a complex topic!
If you only take one thing away from reading this, I’d say when in doubt take a test. Quarantine while you wait for results.
I’d encourage you to purchase a few antigen tests to keep on hand in your home. Remember you can always ask your own doctor for advice about when and how to take a test. You aren’t alone in this decision.
Feel free to drop some questions in the comments too, and I’ll do my best.